Part 7: Political Influences
There is little correlation between NIH funding levels and general disease burden on American society, according to two studies from 1998 and 2011.103 As a federal agency, embedded within the Department of Health and Human Services, political influence is inevitable. This influence, according to sources interviewed for this report, is driven by major universities, top research beneficiaries, and nonprofits that lobby for specific diseases.
Too Much Trend Chasing
NIH research priorities are affected by public opinion and usually reflect an increased awareness of particular diseases. The National Cancer Institute has been the highest-funded NIH institute for some time, largely due to political forces prompting President Nixon’s “War on Cancer.”

More than one interviewee claimed that such funding swings have caused some inefficiency in the long-run, particularly with too much money going to cancer and heart disease, and thus resulting in more, lower-yield research being funded. As mentioned, many other interviewees brought up the tendency of some extramural researchers to pursue fads in their grant applications to increase grant approval odds.
Or Maybe Not Enough Trend Chasing
At other times, the NIH has perhaps been too resistant to public opinion.
Consider March 2020 and the onset of the COVID-19 pandemic in the U.S. While millions of people were infected with a novel virus, Patrick Collison, Silvana Konermann, and Tyler Cowen found that the speed with which the NIH shifted federal funds for COVID-19 research was too slow. Few new projects were being funded and many top scientists were waiting for permission from the NIH to repurpose existing funding for the worst pandemic in modern history.
In April, the trio started a program called Fast Grants, under the auspices of the Mercatus Center at George Mason University. Throughout 2020, Fast Grants raised $50 million and disbursed 260 grants. Each grant application took about 30 minutes to complete, and was approved or rejected within 48 hours by a panel of 20 experts who reviewed more than 6,000 applications. Funded projects include an accurate, saliva-based COVID-19 test, successful clinical trials for a generic drug which might reduce COVID-19 hospitalization rates by 40%, and significant research into long COVID. 32% of grant recipients said their research was accelerated by “a few months,” while 64% of recipients claim they would never have been funded without Fast Grants.104
During the first three months of the pandemic, the NIH spent a mere $2 million on COVID research. One intramural researcher complained, in an interview, that their entire project was defunded for new COVID research.
Still, the NIH has a serious problem with rapidly changing research priorities. In 2020, the agency spent $2.4 billion (5.7% of the total budget) on COVID research, including less than $800 million on clinical research. By January 2022, that figure climbed to $5 billion.105
These might seem like small values, but the NIH's budget is usually determined years in advance. Most of its grants extend over several years. A fixed set of funds are allocated for fellowships and grants. With all this money already being set aside then, it’s probably a fair assumption that only a fraction of the NIH’s discretionary budget can be doled away for a new public health crisis. Directing money in a near-sighted way, too, can ultimately impinge upon long-term research.
The sluggish response of this public health agency to a massive public health problem is a serious cause for concern. With a $40+ billion budget, the NIH should have some latitude for quickly redirecting funds even as, according to one interviewee, many researchers switched their projects to COVID-related aims without informing the NIH of their reprioritization until later.
Lobbying by Universities and Nonprofits
NIH beneficiaries can and do lobby the NIH, the Department of Health and Human Services, and Congress. These expenditures are public record.
In 2020, the NIH received 486 registered lobbyists representing 179 clients. Most clients are disease-related nonprofits, such as the American Lung Association and the Tourette Syndrome Association. Others are broader class advocacy groups, like the AARP and National Nurses United.
Many lobbying clients are universities, particularly those that receive lots of NIH funding. Of the top 50 largest NIH recipients in 2020 (including universities and private labs), 40 institutions106 engaged in lobbying of the NIH through the Association of American Universities or the Association of Public Land Grant Universities.107
Combined, the Association of American Universities108 and the Association of Public Land Grant Universities109 spent $1.4 million on lobbying in 2022, though the expenditure was spread out among a dozen federal agencies.
Research!America is a lobbying group devoted to championing the NIH (and to a lesser degree, other public health agencies).110 In 2020, it spent $3.7 million, almost a third of which went to its five main employees.111 The group is financed by many of the same organizations hiring the other lobbyists, including 133 universities and affiliated institutes112 and most of the top 50 beneficiaries.113 114
United for Medical Research is a similar group that lobbies the NIH on behalf of universities. Its funders include both the Association of American Universities and the Association of Public Land Grant Universities, as well as a handful of other major NIH recipients (Princeton, Vanderbilt, Washington University in St. Louis, Harvard, Johns Hopkins and others), some professional associations (ex. American Association for the Advancement of Science), some single disease advocacy groups (ex. the Alzheimer’s Association), and Johnson & Johnson.115 In 2020, United for Medical Research spent $120,000 on lobbying.116
Though I assume the influence of lobbying is relatively minor, given the small expenditures, lobbying directed at Congressmen may prove more effective. According to a 2014 study by professors from New York University and Columbia University, single-purpose nonprofits have a significant impact on which diseases Congress singles out for research recommendations to the NIH. The study found that lobbying led to a higher likelihood for Congress to put “soft earmarks” in bills, which encouraged the NIH to establish particular funding priorities. The NIH, according to this study, has increased funding on rare diseases between 3-15% as a result.117
Electoral Pressure
Congress appropriates the NIH’s funding, and universities benefit from this funding. Large research universities have tens of thousands of employees, massive endowments, and plenty of influential connections. They are often among the largest and wealthiest employers in Congressional districts. Thus, Congressmen from districts with large universities are likely more prone to support increased funding for the NIH.
Consider Johns Hopkins University**,** the largest recipient of NIH funds in 2020. In 2019, JHU employed 27,300 people and the Johns Hopkins Health System, a nonprofit that oversees multiple hospitals and medical centers, employed an additional 23,470 people. These are the two largest, private employers in the Greater Baltimore area and the 7th Congressional district. 118
The University of California Los Angeles was the fourth-largest recipient of NIH funds in 2020. That year, UCLA had 51,000 employees, making it the fourth largest employer in Los Angeles County, with almost 10,000 more employees than the largest private employer.119
Even if Johns Hopkins and UCLA are not directly giving money to Congressmen, many of their thousands of employees are voters, many donate to political campaigns, and others respond to overtures from academic leaders.
Nearly all of the top NIH beneficiaries have 10,000 or more employees, with the notable exceptions of a few private institutes, like the Fred Hutchinson Cancer Research Center (over 3,500120) and the Research Triangle Institute (almost 6,000121). But the importance of all of these institutions is undoubtedly amplified by their fame and influential leadership.
Other Instances of Influence on the NIH
Numerous interviewees, particularly those with former leadership experience at the NIH, stated that there was distortionary political pressure on NIH operations. They pointed to instances of powerful individuals picking up the phone and calling the right people.
One interviewee said he knew a Congressman who told him: “the NIH is [like the Mafia], and the only time in my life when I’ve been physically threatened is when I proposed reducing NIH funding." The same congressman also referred to the NIH as a “jobs program," at least from a congressional perspective.
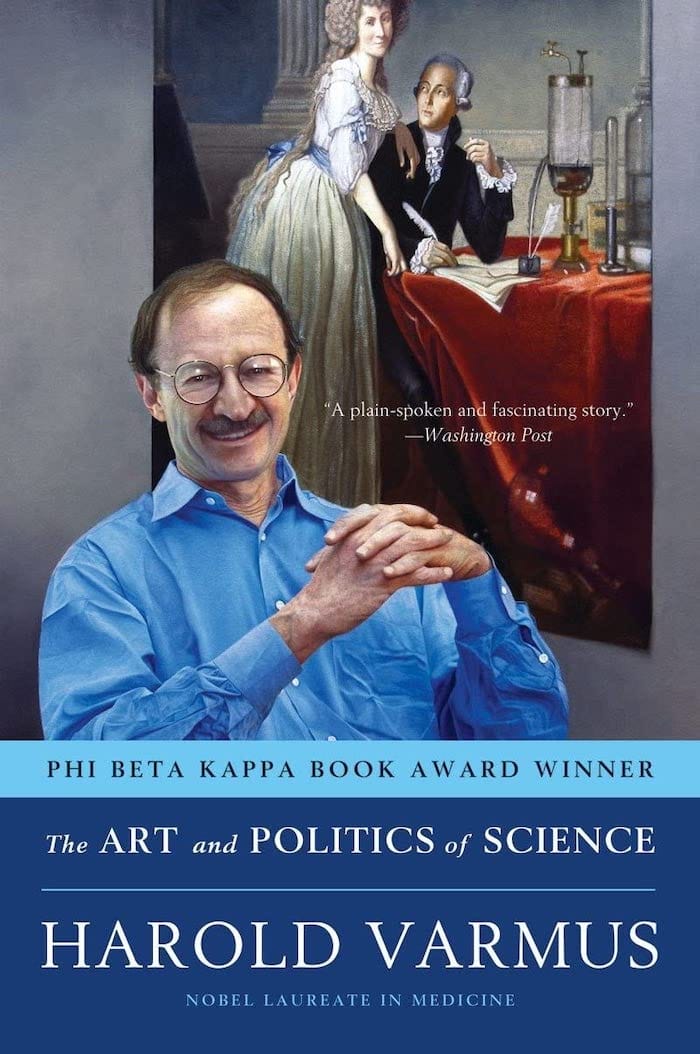
Consider “The Art of Politics and Science,” a 2007 memoir by Dr. Harold Varmus, who served as director of the NIH from 1993-1999, and then as director of the National Cancer Institute from 2010-2015. Varmus describes being beset by special interest groups and politicians, who constantly angled for shifts in the budget to support their hobby horses.122
“One of my first exposures to this problem occurred soon after I arrived at the NIH, when I received a call from my own former congresswoman, Nancy Pelosi, asking me to add $50 million to the budget for AIDS research. As the representative from one of the districts most heavily affected by the epidemic, her wishes were understandable,” Varmus wrote. “I declined as politely as I could.”
Varmus continues:
“Sometimes it was not so easy to say no. Late one afternoon in May of 1996, as I was walking on the NIH campus, my driver pulled up with an urgent expression and asked me to take an emergency call on the car phone. A senior member of the administration—Jack Lew, then deputy director, later director, of the Office of Management and Budget—told me that the president had just met the recently paralyzed actor Christopher Reeve for the first time that afternoon and had promised in the presence of the press to increase spending on spinal cord research by $10 million. I started to explain the difficulties of doing this, when the phone was passed at the other end to a more junior person, who said, basically, just do it, don’t argue, or you won’t get the money. Of course, the White House was not in a position to send us any additional funds directly. But the president’s wishes are always obeyed. When the next accounting was made of disease-specific spending at the neurology institute (formally known as the National Institute for Neurological Diseases and Stroke, or NINDS), the funds for spinal cord research were accordingly higher, and funds for other purposes were proportionately lower.”
Single issue nonprofits, too, are a focus of Varmus' book. Specifically, he writes that advocates often “refuse to recognize, or to care, that funds for their disease must come from funds being spent elsewhere, including funds used for a disease important to another group of advocates.”
In one instance, nonprofit advocates for diabetes research “adopted an unusually militant approach,” Varmus writes, “openly criticizing my management of the NIH and even picketing the Illinois home of John Porter, the chairman of our House Appropriations Subcommittee. (The attack on Porter was ill-conceived: his wife was a diabetic, his concerns about the disease were evident, and his support for the NIH was unsurpassed.) … These groups can limit the possibilities for adjusting the distribution of funds across the institutes, since annual changes in each institute’s budget are scrutinized carefully, to one hundredths of a percentage point, and any downward deviation from the NIH average is likely to result in appeals to influential congressional or administration advocates. This has the sometimes stultifying effect of keeping institute budgets in approximate lockstep, simply to avoid the inevitable outcry if one of them doesn’t do well.”
